2024-04-10
The Most Hated Device in Healthcare Part 1
Unveiling the Past: The Introduction of Electronic Health Records
In this inaugural post of our series, "The Most Hated Device in Healthcare", we take a step back into medical history to uncover the evolution of the Electronic Health Record (EHR)—a tool that sits at the heart of modern healthcare controversy. Dubbed one of the most significant shifts in healthcare management, the transition from paper-based charts to EHRs has not been without its trials and tribulations. This narrative is not merely about technological change; it is about the impact on those at the front lines of medicine.
From the initial convenience of digitized records to the deep-seated frustration with current systems, our journey begins with,"Unveiling the Past: The Evolution of Electronic Health Records". Readers are encouraged to delve into this exploration to build an understanding of why EHRs have become sources of clinician disdain. By contextualizing the EHR within its historical backdrop, we aim to uncover the layers of complexity that have contributed to its contentious presence in healthcare. Join us as we dissect the beginnings, the promises, and the missteps that have led to the current state of EHRs—a foundational knowledge essential for anyone looking to grasp the full picture of healthcare's digital revolution.
This post will set the context of what was the paper chart and the introduction of the electronic health record.
The journey from paper-based charts to digitizing the health record represents one of the most significant transitions in the history of healthcare. This transformation has not only reshaped the administrative landscapes of hospitals and clinics but has fundamentally altered the healthcare professionals’ approach to their jobs. Understanding the evolution of EHRs unveils insights into both the challenges and innovations that have shaped modern healthcare practices.
The Era of Paper Charts
Traditionally, hospitals, doctors, and nurses relied heavily on paper charts to record, store, and manage patient information. Let’s call them PHRs, paper health records for fun. A typical PHR would consist of several sections, each delineated by tabs for quick navigation. These sections might include personal and demographic information, medical history, medication lists, progress notes, lab reports, and diagnostic test results. The front cover or the first page often contained the patient's name, date of birth, and other identifying details for easy reference. Inside, the pages were filled with handwritten notes, lab results, and forms that had been completed by various healthcare providers over time. Often a chalkboard or whiteboard in the room would be used by the nurse to document the medicines that they administered.
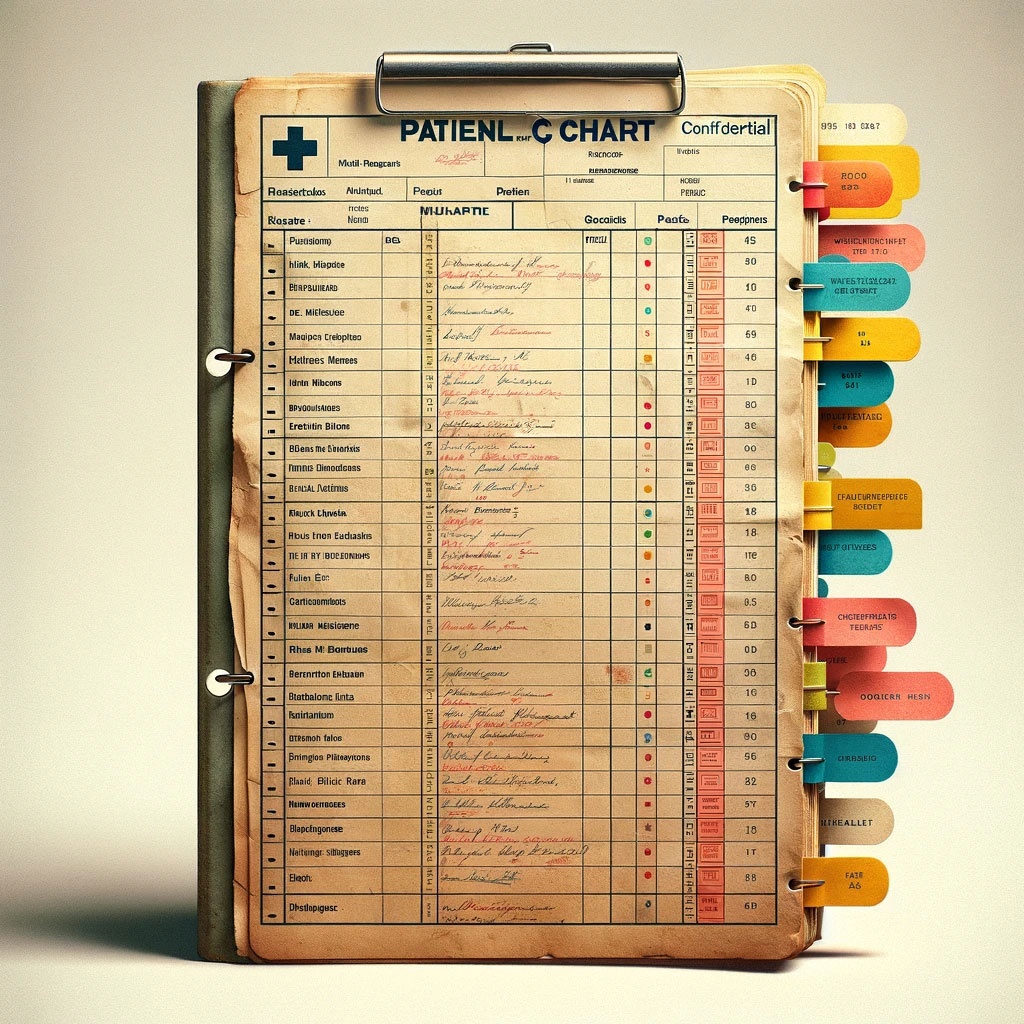
This system, while straightforward, was fraught with limitations and inefficiencies. Paper charts required extensive physical storage space, were prone to damage and loss, and could only be used by one healthcare provider at a time. Moreover, legibility issues with handwritten notes often led to misinterpretations, which would compromise patient care. It was said that the pen was the most dangerous medical device due to these legibility issues. The manual nature of updating and maintaining these records also created significant administrative burdens.
Challenges of a PHR System
Accessibility was a major issue, as retrieving historical patient records was time-consuming and cumbersome. This often led to delays in care, especially in emergencies where swift access to patient histories was critical. A doctor may have picked up a chart and taken it to another floor, or a nurse might have had it while they were doing charting. Visibility of what was happening to the patient was non-existent for many ancillary departments. Physicians would write down orders (on paper) and send them to the pharmacy. If the paper was lost, it might never have been detected.
Once the patient was discharged, the chart would be sent to the medical records department. This department consumed large amounts of space with filing cabinets and shelving filled with patients’ records.
Additionally, the lack of standardization across records made it difficult to track patient outcomes over time and across different healthcare settings. The risk of human error in recording and transcribing information further exacerbated these challenges, leading to potential discrepancies in patient care and treatment plans.
The Clinician Experience
With all these challenges there was a bright spot on the paper chart. The physician could jot down instructions on what he or she wanted for the patient. Simple and straightforward, at least for the physician. The nurse was left to interpret how these instructions should be carried out. The nurse would jot down reminders on a piece of paper some called their brain while others wrote things on the back of their hands. Physicians would get phone calls or pages from pharmacists, nurses, or other staff asking for clarification. Keep in mind this was before cell phones which created delays in care as things would get clarified. The friction in the process was spread mostly downstream from the physician. When a physician got those annoying calls for clarity many times the physician did not see it as a lack of clear direction rather than an inability for others to be autonomous.
Emergence of Electronic Health Records
In the mid-1960s the development of EHRs emerged. They were driven by technological advancements and a growing recognition of the need for more efficient, reliable, and accessible means of managing health information. Early adopters of EHRs were often large healthcare institutions and forward-thinking practitioners who recognized the potential of digital solutions to enhance patient care and operational efficiencies.
Initial Scope and Functionality
The initial scope of EHR functionality focused not only on digitizing patient records to improve accessibility and reliability but also on billing. In the 1970s two major developments were made. Electronic data interchange (EDI) originating in the automotive industry to exchange documents was adapted to healthcare care. Secondly, international classification of diseases, ICD made its ninth major revision (ICD-9) so that billing can be interoperable.
As in all business, following the money will get you to the root of most changes. With the ability to reduce the friction of getting paid, these standards were quickly adopted. To this day billing has the richest discrete data stored in standardized formats. Imagine if there was the same alignment on patient care how different the healthcare industry would be.
These early systems were much simpler than what we have today. Hospitals had a lab system, a radiology system, a pharmacy system, and so on. Each of these systems was closed and didn’t communicate with the others. These systems allowed the ancillaries to increase speed and efficiency. These early systems also enabled healthcare providers to create, communicate, store, and access patient information electronically, thereby addressing some of the limitations of paper-based records.
Conclusion
The slow transition from paper-based charts to Electronic Health Records (EHRs) marked a transformation in healthcare's operational and clinical arenas. In the bygone era of physical charts, healthcare was hindered by the tangible limitations of paper. The cumbersome process of managing voluminous charts, the potential for lost or damaged records, and the ever-present risk of human error posed significant challenges to patient care. The pen once deemed the most dangerous medical device began to replace electronic data.
The standardization of billing information and the ability to exchange data improved the revenue cycle side of providers.
Healthcare has always been complex. Although these simple systems have addressed some problems, they have also left behind many gaps while creating new types of problems to solve. To address these issues, the scope of the EHR needed to be expanded, and expand they did. I will cover this in my next post “Beyond Record-Keeping: The Expanded Influence of EHRs in Healthcare”. We will see why the path of the EHR was on a path to be hated.
In the meantime, I’d love to hear about your experiences with paper charts and or early healthcare IT systems!
Chuck Schneider is a thought leader in healthcare tech. He was one of the original architects of a major EHR and has 11 patents. When he is not thinking about healthcare you can find him outside engaged in some adventure.